More Information
Submitted: December 12, 2024 | Approved: December 27, 2024 | Published: December 30, 2024
How to cite this article: Anderson B, Anderson G. Radiation Safety. J Radiol Oncol. 2024; 8(3): 097-099. Available from:
https://dx.doi.org/10.29328/journal.jro.10010722
DOI: 10.29328/journal.jro.1001072
Copyright License: © 2024 Anderson B, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Radiation Safety
Bradley Anderson1 and Greg Anderson2*
1University of Maryland School of Medicine, Maryland, USA
2Professor, Thomas Jefferson University, Pennsylvania, USA
*Address for Correspondence: Greg Anderson, Professor, Thomas Jefferson University, Pennsylvania, USA, Email: davidgreganderson@gmail.com; Greg.Anderson@rothmanortho.com
Radiation is a form of energy. There are two basic types of radiation: Particulate radiation and Electromagnetic radiation [1].
Particulate Radiation includes alpha particles and beta particles. Particulate radiation is produced by the disintegration of an unstable atom and includes alpha and beta particles. These particles have both energy and mass [1]. Alpha particle are larger subatomic structures involving two protons and two neutrons, which are capable of traveling only short distances with minimal tissue penetration. Alpha particles can, however, cause substantial biologic damage when inhaled or ingested. Beta particles are fast moving electrons (or positrons) and are capable of traveling longer distances, penetrating deep into or through tissue [1]. Beta particles (positrons) are used in Positron Emission Tomography (PET) scans.
The second basic type of radiation is Electromagnetic Radiation (EMR) which includes (in order of increasing energy) radio waves, microwaves, infrared waves, visible light, ultraviolet light, x-rays and gamma rays. EMR is pure energy with no mass and has characteristics of both an electric and magnetic field. EMR is emitted by charged particles and travels in an oscillating wave with a wavelength that is inversely proportional to the energy of the wave. Electromagnetic waves contain photons, or small packets of energy, which travel (in a vacuum) at the speed of light [1].
Ionizing radiation includes forms of radiation that carry enough energy to liberate electrons from atoms, thus ionizing the atom. In the electromagnetic spectrum, wavelengths shorter than visible light are capable of ionizing atoms. Ionizing radiation can exert a major effect on human health by creating damage to DNA and causing genetic mutations. There are many sources of ionizing radiation in the environment including both natural and man-made sources. The average background radiation is world-wide is about 3 mSv (0.3 rem) per year. Natural sources of ionizing radiation account for about 80% of the background radiation to humans and include cosmic radiation, solar radiation, ingestion of radioactive elements, radon gas and ground sources of radiation. Medical radiation accounts for the greatest component of man-made radiation exposure to humans and includes various diagnostic and therapeutic modalities [2].
In an occupational setting, exposure to ionizing radiation should be limited to the greatest extent possible to limit the potential health impacts of radiation exposure. Unfortunately, there is no threshold effect for ionizing radiation exposure, meaning that there is no exposure level, below which, there is zero health risk. The sievert (Sv) is the primary unit utilized to discuss the effects of medical radiation exposure and is defined as 1 joule of energy per kilogram of body tissue, averaged over the whole body. In occupational settings, radiation is generally measured in millisieverts (mSv), or 1/1000 Sv. The effects of ionizing radiation are reduced by the distance from the source according to the inverse square law: intensity = 1/distance [1].
Ionizing radiation has become an indispensable tool in modern medicine. Radiation is used in medicine in two primary ways: to diagnose disease or injury and to kill unwanted (generally cancerous) cells. The oldest and still most commonly used radiation modality is the plain radiograph. In this study, x-rays are passed through body tissues and collected on a photosensitive detector (film), producing an image of the tissues traversed by the x-ray beam. Less commonly performed diagnostic studies, in the field of nuclear medicine, involve the injection, swallowing or inhalation of a radioisotope which emits particles which can be detected (by a gamma camera) for diagnostic purposes [2]. In general, the radioisotope chosen preferentially localizes to the specific tissues or organ where diagnostic information is required.
Due to the potential negative health impact of ionizing radiation, the Federal and State Governments impose strict controls on ionizing radiation exposure in an occupational setting [3]. The two primary bodies which oversee and provide recommendations on occupational exposure limits for radiation include the International Commission on Radiological Protection (ICRP) and The National Council on Radiation Protection (NCRP). In general, the guidelines established by these organizations have two principle objectives: 1) to prevent acute unhealthful radiation exposure; and 2) to limit chronic radiation exposure to “acceptable” levels [1]. The general philosophy of occupational radiation exposure is to maintain exposure levels “as low as reasonable achievable”. This means that all radiation workers should make every reasonable effort to reduce radiation exposure to humans, far below the required limits, whenever possible [1]. When considering diagnostic medical radiation exposure, the primary variables to consider are: exposure time, distance from the source and the presence of shielding [4].
In the United States, the ICRP and NCRP recommendations include [5-7]:
1. Occupational exposures
- Annual effective dose limit: 50 mSv per year
- Cumulative effective dose limit: 10 mSv X age (years)
2. Equivalent dose limits for specific tissues
- Lens of eye: 150 mSv
- Skin, hands, feet: 500 mSv
- Thyroid: 20 mSv
The primary risk from occupational radiation exposure is an increased risk of cancer, although other diseases such as cataracts and teratogenesis are also of concern. The risk depends on the amount of radiation received, the time over which the dose is received, and the body parts exposed. Although scientists assume low-level radiation exposure increases one’s risk of cancer, medical studies have not demonstrated adverse health effects in individuals exposed to small chronic radiation doses (i.e., up to 10,000 mrem above background). Also, the increased risk of cancer from occupational radiation exposure is small when compared to the normal cancer rate in modern society [1].
As mentioned, there is no threshold effect, which means that there is no radiation dose with a zero risk of excess tumor formation. For instance, one study documented an increased rate of DNA translocation and certain cancers in the pilots, which were exposed to radiation from flying at high altitudes [8]. Cancer risk was found to increase with more years of flight, showing the cumulative effects to radiation workers [8].
Among hospital workers, Orthopaedic surgeons have been shown to have as high as a five-fold increased chance of tumor formation, presumably caused by the prolonged occupational exposure to ionizing radiation [3]. The most common modality to expose the Spine Surgeon to radiation is the C-arm used during spinal procedures. Unfortunately, spinal procedures, using fluoroscopy, may expose the surgeon to radiation doses which are 10 to 12 times higher than for other nonspinal musculoskeletal procedures [9].
Patient exposure should also be considered. The relative radiation exposure of common diagnostic imaging modalities [7].
- Lumbar AP and lateral radiograph ⇒ 1.8 mSv
- Percutaneous insertion of 4 pedicle screws ⇒ 0.5 mSv
- Spiral CT scan of chest or abdomen ⇒ 10-20 mSv
- Cardiac ablation procedure ⇒ 10-300 mSv
As mentioned above, radiation exposure to the cornea can cause cataracts. Cataract formation is 4.6 times more frequent in radiation workers compared with nonradiation workers [10]. One study involving kyphoplasty found that radiation exposure to the eye was 0.271 ± 0.200 mSv per vertebra when eye shields were not used [11].
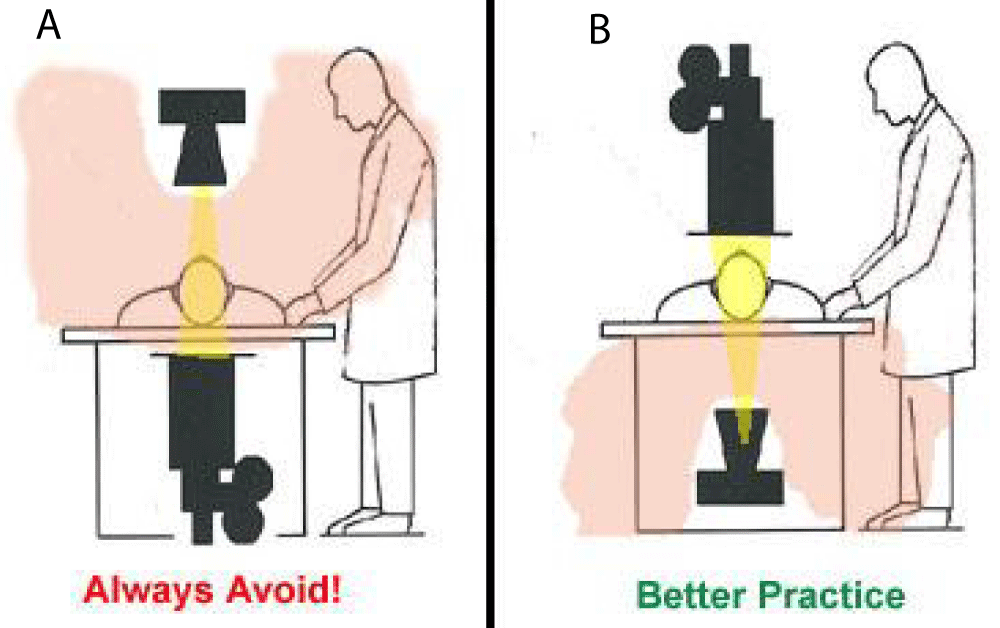
Radiation scatter from the x-ray beam hitting the patient, metal retractors and the OR table is the primary source of radiation exposure to the surgeon. The dose of radiation scatter is much higher on the side of the x-ray emitter as compared to the receiver (Figure 1). To minimize the effects of radiation exposure, the following steps should be taken [12]:
Figure 1: Shows the largest amount of scatter radiation is produced where the x-ray beam enters the patient: A. Position the X-ray tube under the patient not above the patient, B. By positioning the x-ray tube below the patient, you decrease the amount of scatter radiation that reaches your upper body.
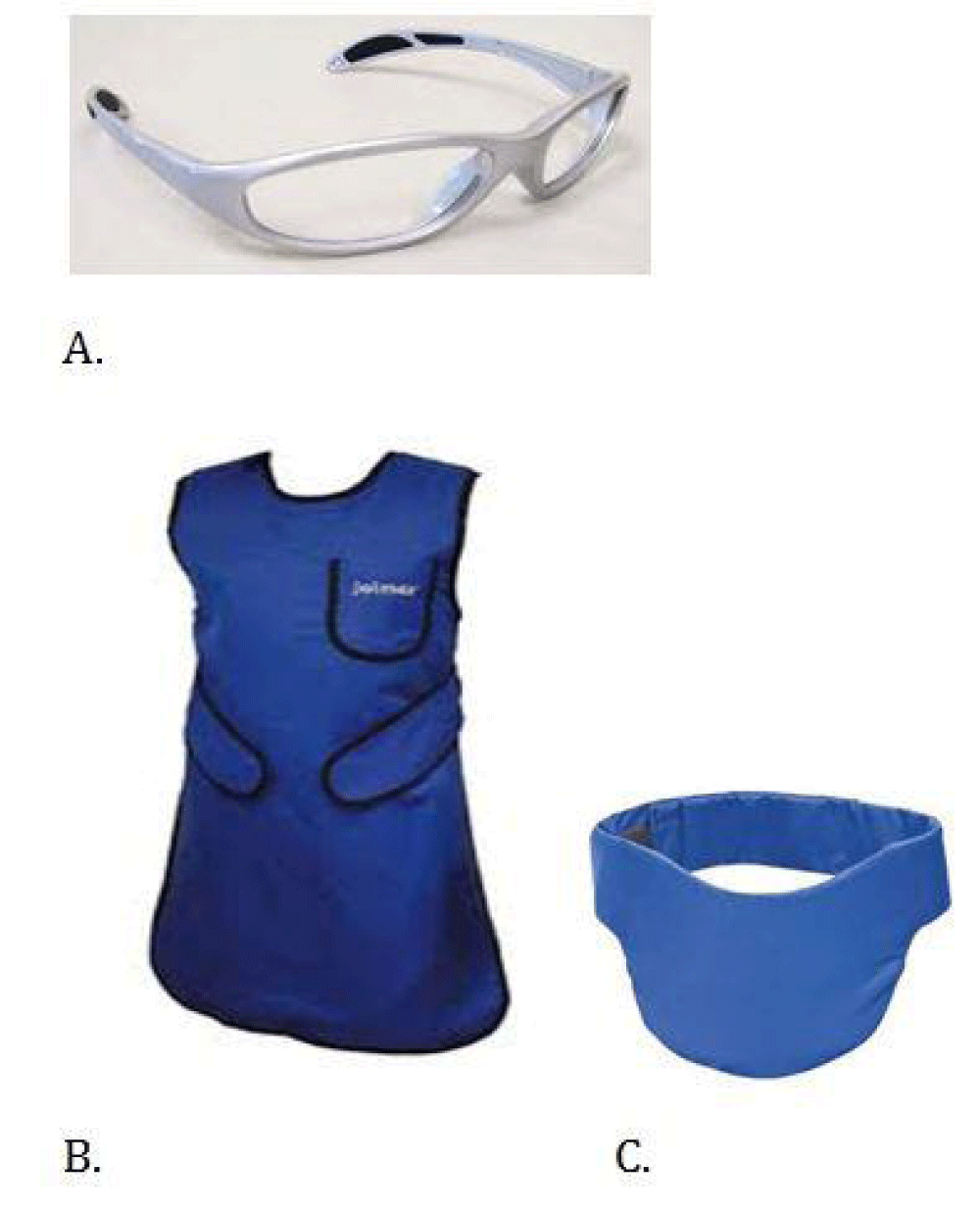
1. Shielding: The surgical team should used personal protective equipment in operating room (Figure 2).
Figure 2: Shows personal protective equipment used in operating room: A. Leaded glasses (0.75 mm of lead equivalent), B. Leaded apron (0.5 mm of lead equivalent), C. Thyroid shield (0.5 mm of lead equivalent).
2. Distance: As dictated by the inverse square law, the exposure to radiation is inversely proportional to the square of the distance to the source. Therefore, the surgeon and other personnel should be located as far away as practical from the radiation source during fluoroscopic procedures [12]. When possible, the surgeon should work on the side of the x-ray source and not the x-ray emitter.
3. Fluoro time: Minimize the beam-on time when using fluoroscopy. Use good coning techniques to narrow the beam and avoid magnification mode which has a higher radiation output. Use spot images, rather than using continuous fluoroscopic images whenever possible [12,13].
Understanding the physics of radiation and the biologic effects of radiation exposure, a surgeon can minimize the health risks to himself/herself and reduce the risks to the surgical team and patient. Proper personal protective equipment should always be utilized and specific steps should be taken to reduce fluoroscopic time and increase the distance from the radiation source when performing spinal procedures.
- NDT Education Resource Center. The Collaboration for NDT Education, Iowa State University. 2001-2012. Available from: https://www.cnde.iastate.edu/nde-education/ndt-resource-center/
- IAEA. Available from: https://www.iaea.org/Publications/Booklets/Radiation/radsafe.html
- ISIS Annual Meeting Radiation Safety for the Spine Interventionalis. Available from: https://www.gehealthcare.com/
- Grover SB, Kumar J. A review of the current concepts of radiation measurement and its biological effects. Indian j Radiol Imaging. 2002;12:21-32. Available from: https://inis.iaea.org/search/search.aspx?orig_q=RN:33035091
- Balter S. An overview of radiation safety regulatory recommendations and requirements. Catheter Cardiovasc Interv. 1999;47:469-474. Available from: https://doi.org/10.1002/(sici)1522-726x(199908)47:4%3C469::aid-ccd18%3E3.0.co;2-x
- Giordano BD, Baumhauer JF, Morgan TL, Rechtine GR. Cervical spine imaging using standard C-arm fluoroscopy. Spine. 2008;33:1970-1976. Available from: https://doi.org/10.1097/brs.0b013e31817e69b7
- Jone DP, Robertson PA, Lunt B, Jackson SA. Radiation exposure during fluoroscopically assisted pedicle screw insertion in the lumbar spine. Spine. 2000;25:1538-1541. Available from: https://doi.org/10.1097/00007632-200006150-00013
- Young LC, Sigurdson AJ, Ward EM, Waters MA, Whelan EA, Petersen MR, et al. Increased frequency of chromosome translocations in airline pilots with long-term flying experience. Occup Environ Med. 2009;66(1):56-62. Available from: https://doi.org/10.1136/oem.2008.038901
- Kim CW, Lee YP, Taylor W, Oygar A, Kim WK. Use of navigation-assisted fluoroscopy to decrease radiation exposure during minimally invasive spine surgery. Spine J. 2008;8(4):584-90. Available from: https://doi.org/10.1016/j.spinee.2006.12.012
- Milacic S. Risk of occupational radiation-induced cataract in medical workers. Med Lav. 2009;100(3):178-86. Available from: https://pubmed.ncbi.nlm.nih.gov/19601402/
- Mroz TE, Yamashita T, Davros WJ, Lieberman IH. Radiation exposure to the surgeon and the patient during kyphoplasty. J Spinal Disord Tech. 2008;21(2):96-100. Available from: https://doi.org/10.1097/bsd.0b013e31805fe9e1
- Radiologic Science for Technologists: Physics, Biology and Protection: 4th Edition. Stewart Bushong.
- Mastrangelo G, Fedeli U, Fadda E, Giovanazzi A, Scoizzato L, Saia B. Increased cancer risk among surgeons in an orthopaedic hospital. Occup Med (Lond). 2005;55(6):498-500. Available from: https://doi.org/10.1093/occmed/kqi048