More Information
Submitted: July 12, 2023 | Approved: August 21, 2023 | Published: August 22, 2023
How to cite this article: Idrees H, Zarrar R, Mujtaba B. Retroperitoneal Bronchogenic Cyst: Imaging and Pathophysiological Review. J Radiol Oncol. 2023; 7: 042-046.
DOI: 10.29328/journal.jro.1001051
Copyright License: © 2023 Idrees H, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Retroperitoneal bronchogenic cyst; Computed tomography; Magnetic resonance imaging; Bronchogenic cyst
Retroperitoneal Bronchogenic Cyst: Imaging and Pathophysiological Review
Hajra Idrees, MBBS1* , Raza Zarrar, MBBS, MD2
, Raza Zarrar, MBBS, MD2 and Bilal Mujtaba, MD1
and Bilal Mujtaba, MD1
1Department of Radiology, University of Texas MD Anderson Cancer Center, Houston, Tx, USA
2Department of Internal Medicine, Baptist Hospitals of Southeast Texas, Beaumont, Tx, USA
*Address for Correspondence: Hajra Idrees, MBBS, Department of Radiology, University of Texas MD Anderson Cancer Center, Houston, Tx, USA, Email: HIdrees@mdanderson.org
Bronchogenic cysts are rare lesions that form during early embryogenesis and are commonly located in the mediastinum. Retroperitoneally located bronchogenic cysts are an exceptionally rare entity. These are most commonly found incidentally on imaging. We will review the unique imaging and histopathological findings of this entity and discuss why prophylactic surgery is considered the treatment of choice. By reviewing retroperitoneal bronchogenic cysts, we aim to educate clinicians regarding the presentation, investigations, imaging characteristics, and treatment of this exceeding rare entity.
Bronchogenic cysts are infrequently occurring lesion that originates primarily from the primitive foregut between the 3rd and 7th weeks of embryonic development. This malformation of the lower respiratory tract is usually found in the thoracic cavity; however, it can rarely occur in the abdominal and pelvic cavity. A study published in 2012 documented only 62 cases of bronchogenic cysts which makes it a rare entity according to modern literature. From our literature review, most of the work on this rare entity is in the form of case reports, which makes a comprehensive review article very important. This cyst is hypothesized to result from an anomaly during the budding of the primitive bronchial tree and is presumed to be benign in the vast majority of cases. The retroperitoneal location of a bronchogenic cyst is an exceedingly rare occurrence. Bronchogenic cysts initially gained the attention of Meyer, et al. in 1859, whereas their retroperitoneal location was discovered in 1953 by Miller, et al. Our review aims to educate our audience regarding the origin, presentation, differential diagnosis, workup including laboratory testing, and most importantly imaging, treatment, and prognosis of this rare entity. [1-4].
Embryogenesis
Bronchogenic cysts are thought to result from an abnormality during embryogenesis. These cysts are a rarely occurring entity that originates primarily from the primitive foregut during weeks 3-7 during embryonic development. The exact pathogenesis remains unknown; however, several hypotheses do exist. To understand these hypotheses a basic understanding of the embryogenesis is required. The development of the lungs begins in weeks 3-4 of embryogenesis leading to the formation of the primitive gut tube. Subsequently, during weeks 4-5 the respiratory diverticulum out pouches from the foregut, forming the primitive lung buds. By the end of week 7, the two bronchopulmonary buds form that will become the adult lungs. During weeks 4-7 the primitive diaphragm undergoes its formation starts leading to the separation of the coelomic cavity into the superior thoracic, and the inferior abdominal segments resulting in partitioning of the abdominal from the thoracic cavity. During week 7, the ventrally growing transverse membranes will eventually fuse with the septum transversum, therefore finally sealing the pericardioperitoneal canals. The left canal is not only larger but also closes later in comparison to the right canal. That is the reason why retroperitoneal bronchogenic cysts are thought to be more common on the left side of the abdominal cavity [2,5].
The first hypothesis for the formation of retroperitoneal bronchogenic cyst is that it is a foregut duplication cyst originating from within the abdomen or retroperitoneum and therefore found in the vicinity of primitive foregut derived such as the pancreas, liver, and stomach. Secondly, in 1985 Sumiyoshi, et al. theorized that bronchogenic cysts are congenitally abnormal budding from the respiratory epithelium. This hypothesis is distinct because it proposed two separate mechanisms that are based on the eventual location of the cyst. Bronchogenic cysts surrounding structures derived from the primitive foregut, namely the tracheobronchial tree, and esophagus, may have developed whilst attachment to the foregut persisted. In contrast, if the cyst is found within or below the diaphragm, it may be due to the abnormal lung buds being pinched off the developing tracheobronchial tree before the closure of the diaphragm [2,5,6].
Demographic
Retroperitoneal bronchogenic cyst is found equally in both men and women with the age of presentation being as young as 25 weeks of gestation and up to a 59-year-old. A majority of these cysts are found on the left side of the abdominal cavity with a typical size at the time of presentation being less than 5 cm in diameter, although lesions measuring up to 18 cm have been reported. As discussed earlier the lung and the esophagus share the same primary embryonic organ, namely the primitive foregut, therefore it is understandable that up to 80% of bronchogenic cysts occur above the diaphragm. Rarely, these lesions are seen below the diaphragm which is the topic of this review. Retroperitoneal bronchogenic cysts similarly being a derivative of the tracheobronchial bud that originates from the primitive foregut, also tend to surround organs that are derived from the proximal gut. The most common location for retroperitoneal bronchogenic cysts is surrounding the left adrenal gland, head, and body of the pancreas, followed by the kidney. These cysts tend to be located within a triangle bordered medially by the sagittal plane, inferiorly by the splenic vein, and superiorly by the diaphragm [1,3,4,6-8].
Presentation
Retroperitoneal bronchogenic cysts are largely asymptomatic and thus a majority are found incidentally on imaging. If present, symptoms are commonly caused by the cyst compressing surrounding structures. Patients may present with nausea, vomiting, abdominal pain, early satiety, fever, perforation, hemorrhage, intestinal obstruction, or pheochromocytoma-like symptoms. Symptomatic patients tend to be older as a result of the expansion of the cyst due to epithelial secretions, resulting in compression of surrounding structures. One study found that most symptomatic patients have a larger cyst, measuring over 7 cm in diameter at the time of diagnosis [1,5,8].
Differential diagnosis
Retroperitoneal bronchogenic cysts are an incidental finding on imaging in the vast majority of cases. Formulating a broad differential diagnosis is very important for a multitude of reasons. Firstly, the location of the retroperitoneal bronchogenic cyst being in the abdominal cavity and thus alongside numerous vital organs can cause significant concern for compression, malignancy, or invasion of any of these viscera that could be determinantal to the patient. Lastly, as we will learn later in the review the definitive diagnosis can only be reached on postsurgical histopathology, therefore a broad differential diagnosis followed by an efficient workup is essential. Differential diagnosis includes benign and malignant tumors, metastatic lesions, cystic lesions, infections, teratomas, and bronchopulmonary sequestrations of the abdominal cavity. The most notable benign lesions include adrenal adenoma, ganglioneuroma, stromal tumors, lipoma, lymphangioma, and pseudopapillary neoplasms. More concerning are the malignant lesions that include pheochromocytoma, adrenal cortical carcinoma, pancreatic neoplasms, soft tissue neoplasm of the retroperitoneum, sarcoma, and lymphoma. Cystic lesions include the adrenal, retroperitoneal, esophageal, pancreatic, mucinous, undifferentiated foregut, epidermoid, tailgut, enteric, and dermoid cysts, in addition to cystic degenerated adenoma, pancreatic pseudocysts, cystic lymphangioma, cystic mesothelioma and, cysts of foregut and urogenital origin. Lastly, a rare yet concerning infection that should be considered is adrenal tuberculosis [2,3,5,7].
Bronchogenic cysts are derived from mesodermal and endodermal layers during embryogenesis which makes them display a variety of patterns that are not dissimilar to cystic teratomas. Teratomas can potentially undergo malignant transformation, therefore must be differentiated and removed. Cystic teratomas will contain all 3 layers, including mesoderm, endoderm, and ectoderm which can be seen on imaging and definitively diagnosed on histopathological analysis. The last differential diagnosis which can be considered is bronchopulmonary sequestration. This will contain mature lung parenchyma and pleural structures along with bronchial element which is unlike bronchogenic cyst [2,3,5,7,9].
Biochemical tests
Biochemical investigations are an essential part of the diagnosis of any mass presenting in the abdominal cavity. Despite presenting with normal biochemical workup, retroperitoneal bronchogenic cysts require extensive testing as it is commonly found in close proximity to organs known for critical pathologies, such as the pancreas and adrenal glands. Blood investigations include serum potassium, cortisol, basal adrenocorticotropic hormone, metanephrine, normetanephrine levels, and dexamethasone suppression test. Urine can be tested for 24-hour cortisol and catecholamine levels constituting epinephrine, metanephrine, vanillylmandelic acid, and dopamine. These tests would enable investigators to exclude cortisol-producing adrenal adenoma and pheochromocytoma. If the location of the cyst is peripancreatic; pancreatic enzymes such as amylase and lipase levels are essential. Urine and plasma serotonin and 5 Hydroxyindoleacetic acid are needed to rule out carcinoid tumors [3,5].
Tumor markers are an essential part of the workup of retroperitoneal bronchogenic cysts. These include Cancer Antigen 19-9, Beta Human Chorionic Gonadotropin, Alpha-Fetoprotein, and Carcinoembryonic Antigen (CEA). Elevated levels of CEA could be misleading, as it is a normal component of bronchial mucus and can occasionally leak from the cyst. This could raise concern for colorectal cancer, however considering the presence of an abdominal cyst and elevated CEA, it rather aids in the diagnosis of a retroperitoneal bronchogenic cyst [3,5].
Radiology
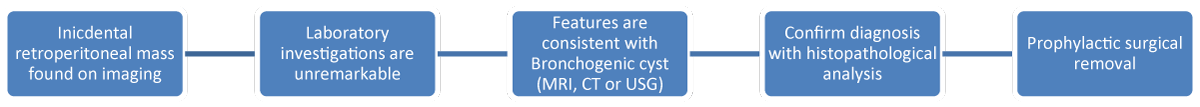
A retroperitoneal bronchogenic cyst is most commonly found incidentally on imaging (Figure 1). This is partially due to an overall surge in the use of imaging in healthcare, in addition to retroperitoneal bronchogenic cyst being asymptomatic at the time of presentation. Ultrasonography (US), computed tomography (CT) scan and magnetic resonance imaging (MRI) are proven imaging modalities that are used to diagnose retroperitoneal bronchogenic cysts. Furthermore, MRI with multidetector CT scan is considered the optimal combination to diagnose this entity. The main purpose of imaging is to narrow down the differential diagnosis based on radiological features, pre-operative surveillance, and identifying invasion into surrounding structures. Radiological features to note are location, neighboring structures, shape, size, wall thickness, calcifications, septa, and fat content of the lesion. A definitive diagnosis maybe be difficult to reach when cysts are too large, compress on adjacent structures, or are infected. In those cases a global approach combining histopathological, radiological, and clinical evidence is optimal [1-3].
Figure 1: Flow chart for diagnosis and management of retroperitoneal bronchogenic cyst.
Computed tomography scan
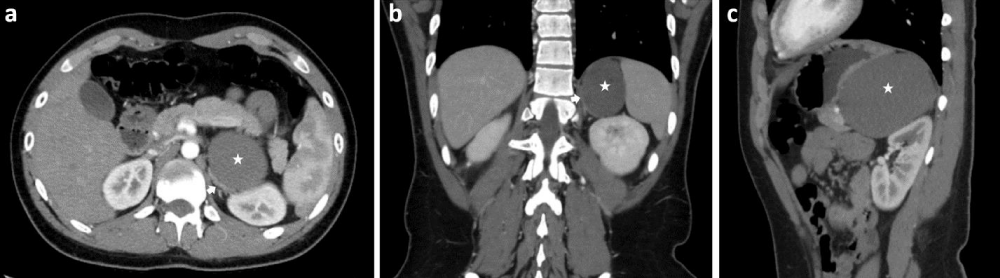
CT scans are more frequently the first imaging modality owing to their faster image acquisition. Retroperitoneal bronchogenic cyst presents as homogenously hypoattenuating, non-enhancing, sharply defined spherical lesions with well-circumscribed smooth or lobulated borders (Figure 2). Retroperitoneal bronchogenic cysts normally contain water and proteinaceous mucus, with possible remnants of prior hemorrhage or infection. This leads to attenuation that is more comparable to that of water (0-20 HU) following intravenous contrast. However, the cyst may contain thick mucinous or proteinaceous secretions, active hemorrhage, or calcification, that will result in hyperattenuation with coefficients of up to 120 HU. This hyper attenuation may result in the cyst being misdiagnosed as a solid structure. Occasionally a fluid-fluid level may form as a result of the higher viscosity fluid settling at the bottom of the cyst. Overall a complete adrenal structure, fusiform appearance, and calcification within a cystic lesion in the adrenal region are indicative of a retroperitoneal bronchogenic cyst. Unfortunately, a CT scan alone may not be able to provide adequate information regarding lesions that lack internal heterogeneity or mural enhancement [1,2,5].
Figure 2: Contrast enhanced CT of the abdomen in the axial (a), coronal (b) and sagittal (c) planes showing a left retroperitoneal suprarenal cyst (star) pushing the left kidney posteroinferiorly, the left adrenal gland (a, b; white arrow) medially, and the stomach superoanteriorly. The cyst is adjacent to the left adrenal gland, pancreas, and stomach. There is no fat tissue between them.
Magnetic Resonance Imagining
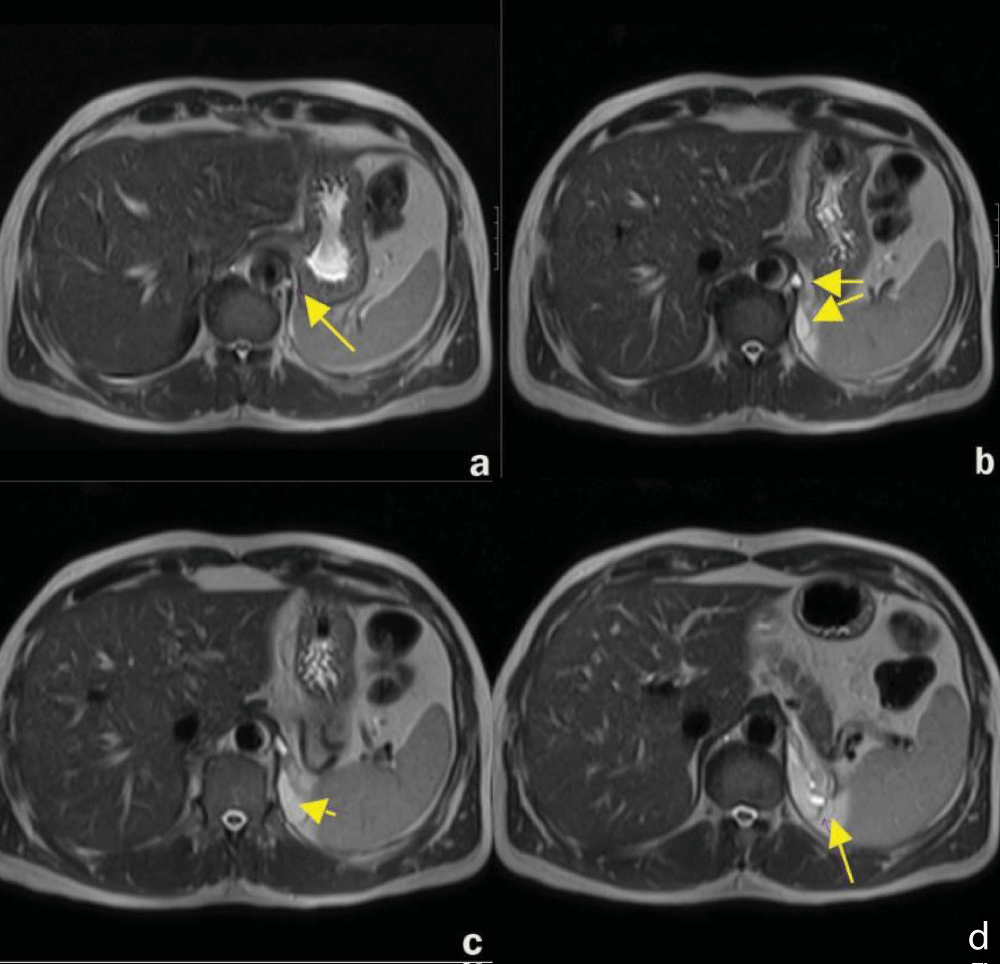
MRI is usually performed after an initial CT scan to provide additional details about the cyst and its surrounding structures. The retroperitoneal bronchogenic cyst has variable signal intensity on MRI (Figure 3). Simple cysts will typically display a very low signal intensity on T1-weighted imaging. Higher signal intensities may be seen because of paramagnetic entities including protein or methemoglobin resulting from hemorrhage which can be suspended in the cystic fluid. The retroperitoneal bronchogenic cyst will typically produce variable intermediate-to-high signal intensity lesions on T1-weighted images. However, based on the contents of the retroperitoneal bronchogenic cyst, it may mimic a solid mass on CT and T1-weighted MRI imaging. As a result, T2-weighted MRI imaging is required, generating an extremely high signal intensity. It is also noteworthy that retroperitoneal bronchogenic cysts can be used to distinguish retroperitoneal bronchogenic cysts from teratoma based on their lack of signal intensity inversion on T1-weighted fat-suppressed imaging [1-3,5].
Figure 3: Magnetic Resonance imaging of the abdomen in axial plane (a-d) showing a retroperitoneal bronchogenic cyst [5].
Ultrasonography
Lastly, ultrasonography is also an effective modality to detect retroperitoneal bronchogenic cysts. Ultrasound is particularly helpful in distinguishing the nature of the cysts. Variable internal echogenicity is apparent, typically presenting as an anechoic lesion with possible hyperechoic debris. Ultrasonography is particularly useful in visualizing well-transduced or calcified cysts. Unfortunately, two major limiting factors have led to the ultrasound falling out of favor. There is interference from gases within the gastrointestinal tract obstructing the view as well as the retroperitoneal space is not easily accessible by ultrasonography [1,2,5].
Pathology
A definitive diagnosis of retroperitoneal bronchogenic cysts can only be made on histopathological analysis (Figure 1). Histologically, bronchogenic cysts are defined as the simultaneous presence of ciliated respiratory epithelium, mucinous glands, and well-differentiated cartilage.
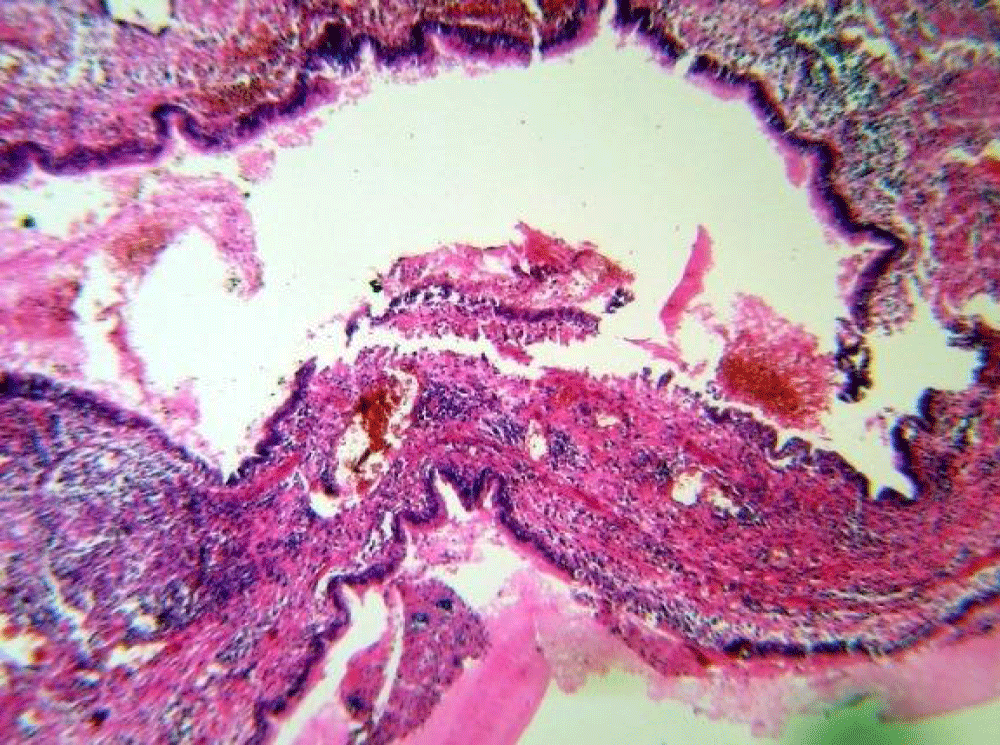
Occasionally, smooth muscle cells may also be present. These cysts are lined by secretory respiratory epithelium ciliated pseudostratified or tall columnar epithelium with bronchial glands, cartilage, thin bundles of smooth muscle, and mucoid material. Cysts lined by pseudostratified ciliated columnar epithelium the differential diagnosis includes, bronchopulmonary sequestration, cysts of urothelial and foregut origin, and cystic teratoma (Figure 4). That is the reason why an accurate pathological diagnosis of this lesion requires combined evaluation of the epithelial lining, and the structures composing the cystic wall. It is noteworthy that infection or malignant degeneration may interfere with the aforementioned diagnostic criteria [1,3,5,7,10,11].
Figure 4: Microscopic section of the bronchogenic cyst showing cystic cavities lined by pseudostratified cylindrical epithelium on a thick fibrous wall containing cartilage, seromucous glands, smooth muscle fascicles and extensive foci of mononuclear inflammatory cells aggregates [11].
Macroscopically, retroperitoneal bronchogenic cysts that are found in proximity to the adrenal glands may appear fusiform in structure due to the growth of the ectopic lung bud on both ends of the blind side of the cyst. This may be due to cyst walls typically containing cartilage, coupled with the narrow spindle-shaped space wedged between the retroperitoneal adrenal regions [2].
Treatment
Prophylactic surgical removal of the retroperitoneal bronchogenic cyst is considered stand of care (Figure 1), provided the patient is a good surgical candidate. This is due to a multitude of reasons, including possible infection of the cyst, misdiagnosis, and subsequent malignant degeneration of the cyst. Removal of an infected cyst can result in an increased rate of surgical compilations and worse outcomes overall. Establishing a definitive diagnosis is virtually impossible without postsurgical histopathological evaluation. There is a possibility of missing the diagnosis of a malignant lesion which could be significantly detrimental to the patient. Malignant degeneration is a rare complication of bronchogenic cysts in the thoracic cavity, first reported by Womack and Graham in 1941. This is thought to arise from metaplastic changes in the lining of the cyst. One case has been reported of a retroperitoneal bronchogenic cyst undergoing malignant degeneration into an adenocarcinoma. Additional malignancies arising through this mechanism may also include bronchioalveolar carcinoma and malignant melanoma. The risk of malignancy is increased in maldeveloped lungs and smokers [8,12,13].
Laparoscopic removal is considered the standard treatment modality utilizing smaller incisions, resulting in shorter hospital stays, fewer postoperative complications, and lower surgical costs. However, due to the malignant potential of the lesion, an endoscopic retrieval bag is key. Surgical removal of the retroperitoneal bronchogenic cyst may be guided by an array of factors, including the location and nature of the lesion. Lesions that are latched on to neighboring viscera may require an en-bloc resection with possible organ removal. Additional novel techniques combatting these lesions also include retroperitoneoscopy, given its advantage of being minimally invasive. Cauterization of residual cyst wall via electrocoagulation is considered when the cyst adheres to neighboring structures. This is done to prevent recurrence of the cyst. Lesions lying in close proximity to the adrenal gland will typically be resected via laparoscopic adrenalectomy. Retroperitoneal excision provides an excellent alternative. This modality poses minimal intraperitoneal adhesion formation risk, alongside being a less invasive, safe, and effective technique that avoids the need for visceral mobilization [2-5].
Fortunately, there have been no reports of recurrence after surgical removal of these cysts. Therefore, complete resection of the retroperitoneal bronchogenic cyst offers a favorable prognostic profile [1].
The retroperitoneal bronchogenic cyst is a rare entity of embryologic origin. Strong clinical suspicion for this cyst should arise if a retroperitoneal lesion is incidentally found on imaging. CT scan combined with MRI is considered the imaging modality of choice. If the imaging is characteristic of a retroperitoneal bronchogenic cyst, this should prompt a histopathological evaluation since the pathology is the gold standard for a definitive diagnosis of this lesion. Prophylactic surgical removal is the standard of care, especially considering the malignant potential of the lesion.
- Hu BY, Yu H, Shen J. A retroperitoneal bronchogenic cyst clinically mimicking an adrenal mass: three case reports and a literature review. J Int Med Res. 2022 Jan;50(1):3000605211072664. doi: 10.1177/03000605211072664. PMID: 35023387; PMCID: PMC8785309.
- Wen Y, Chen W, Chen J, He X. Retroperitoneal bronchogenic cyst resembling an adrenal tumor: two case reports and literature review. J Int Med Res. 2020 May;48(5):300060520925673. doi: 10.1177/0300060520925673. PMID: 32436418; PMCID: PMC7243399.
- Runge T, Blank A, Schäfer SC, Candinas D, Gloor B, Angst E. A retroperitoneal bronchogenic cyst mimicking a pancreatic or adrenal mass. Case Rep Gastroenterol. 2013 Oct 5;7(3):428-32. doi: 10.1159/000355879. PMID: 24403880; PMCID: PMC3884166.
- Cowan S, Gunawardene A, Davenport E. Retroperitoneal bronchogenic cyst mistaken as an adrenal adenoma. ANZ J Surg. 2021 Jul;91(7-8):E526-E527. doi: 10.1111/ans.16515. Epub 2020 Dec 18. PMID: 33336493.
- Govaerts K, Van Eyken P, Verswijvel G, Van der Speeten K. A bronchogenic cyst, presenting as a retroperitoneal cystic mass. Rare Tumors. 2012 Jan 2;4(1):e13. doi: 10.4081/rt.2012.e13. Epub 2012 Mar 20. PMID: 22532911; PMCID: PMC3325740.
- Sumiyoshi K, Shimizu S, Enjoji M, Iwashita A, Kawakami K. Bronchogenic cyst in the abdomen. Virchows Arch A Pathol Anat Histopathol. 1985;408(1):93-8. doi: 10.1007/BF00739965. PMID: 3933174.
- Onol FF, Baytekin F, Dikbas O, Ergönenç T, Tanidir Y. A retroperitoneal bronchogenic cyst mimicking adrenal tumour in an adult: is differential diagnosis truly possible? J Clin Pathol. 2009 Feb;62(2):187-9. doi: 10.1136/jcp.2008.061077. PMID: 19181637.
- Haddadin WJ, Reid R, Jindal RM. A retroperitoneal bronchogenic cyst: a rare cause of a mass in the adrenal region. J Clin Pathol. 2001 Oct;54(10):801-2. doi: 10.1136/jcp.54.10.801. PMID: 11577133; PMCID: PMC1731290.
- Bagolan P, Bilancioni E, Nahom A, Trucchi A, Inserra A, Neri M, Spina V, Giorlandino C. Prenatal diagnosis of a bronchogenic cyst in an unusual site. Ultrasound Obstet Gynecol. 2000 Jan;15(1):66-8. doi: 10.1046/j.1469-0705.2000.00022.x. PMID: 10776016.
- Yang DM, Jung DH, Kim H, Kang JH, Kim SH, Kim JH, Hwang HY. Retroperitoneal cystic masses: CT, clinical, and pathologic findings and literature review. Radiographics. 2004 Sep-Oct;24(5):1353-65. doi: 10.1148/rg.245045017. PMID: 15371613.
- Mirsadeghi A, Farrokhi F, Fazli-Shahri A, Gholipour B. Retroperitoneal bronchogenic cyst: a case report. Med J Islam Repub Iran. 2014 Jul 13;28:56. PMID: 25405122; PMCID: PMC4219886.
- Sullivan SM, Okada S, Kudo M, Ebihara Y. A retroperitoneal bronchogenic cyst with malignant change. Pathol Int. 1999 Apr;49(4):338-41. doi: 10.1046/j.1440-1827.1999.00869.x. PMID: 10365854.
- Azizkhan RG, Crombleholme TM. Congenital cystic lung disease: contemporary antenatal and postnatal management. Pediatr Surg Int. 2008 Jun;24(6):643-57. doi: 10.1007/s00383-008-2139-3. Epub 2008 Apr 5. PMID: 18392629.