Research Article
Diagnostic accuracy of Magnetic Resonance Imaging to differentiate benign and Malignant Parotid Gland Tumors

Sadia Ali1, Adeena Khan2*, Kiran Sarfaraz3, Saba Akram4, Mariam Javaid5 and Asma Bano6
1FCPS Radiology Avicenna Medical College and Hospital, Pakistan
2FCPS, FRCR, MMED, King Abdul Aziz University Hospital, Kingdom of Saudi Arabia
3FCPS Radiology, Lahore General Hospital, Pakistan
4FCPS Radiology, Avicenna Medical College and Hospital, Pakistan
5FCPS Radiology, Avicenna Medical College and Hospital, Pakistan
6FCPS Radiology, Bugshan Hospital, Jeddah, Kingdom of Saudi Arabia
*Address for Correspondence: Dr. Adeena Khan, FCPS, FRCR, MMED, King Abdul Aziz University Hospital, Kingdom of Saudi Arabia, Tel: 00966-599720990; Email: khan.adeena@yahoo.com
Dates: Submitted: 09 October 2018; Approved: 06 November 2018; Published: 07 November 2018
How to cite this article: Ali S, Khan A, Sarfaraz K, Akram S, Javaid M, et al. Diagnostic accuracy of Magnetic Resonance Imaging to differentiate benign and Malignant Parotid Gland Tumors. J Radiol Oncol. 2018; 2: 080-086. DOI: 10.29328/journal.jro.1001026
Copyright License: © 2018 Ali S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Magnetic resonance imaging; Parotid gland tumours; Diagnostic accuracy; Histopathology
Abstract
Objective: To determine the diagnostic accuracy of Magnetic Resonance Imaging (MRI) to differentiate Benign and Malignant Parotid Gland Tumors taking histopathology as gold standard.
Design: Cross sectional study.
Place and duration of study: Department of Diagnostic Radiology, Lahore General Hospital, Lahore from January till July 2014.
Methodology: 200 patients of age between 5 to 80 years of either gender with parotid gland swelling, having radiological evidence and clinical suspicion of parotid tumour like fixation to underlying skin, pain, facial palsy and cervical lymphadenopathy were taken. T1 and T2 plain and contrast enhanced 1.5 Tesla MRI unit using standard imaging coil was then carried out. Imaging was further evaluated for the presence or absence of benign or malignant parotid gland tumours using histopathology as a Gold standard. Sensitivity, specificity, positive predictive value, negative predictive value and diagnostic accuracy of MRI were taken against the gold standard.
Results: There were 170 males and 30 females having mean age of 40.27±15.04 and 40.12±12.15 years respectively. Sensitivity, specificity, positive predictive value and negative predictive value of MRI were 90.4%, 89.33%, 93.39% and 84.41% respectively. The diagnostic accuracy of MRI to differentiate benign and malignant parotid gland tumours was 90%. These results were taken against surgery histopathology as a gold standard.
Conclusion: MRI is highly accurate in differentiating malignant & benign tumours of parotid glands and can be used as an adjunct to histopathology for pre-operative evaluation of the parotid gland tumours.
Introduction
Salivary gland tumours constitute 3% of all head and neck tumours. Out of the parotid gland tumours account for 80%. Female to male ratio is 1.04: 1 with mean age of 47 years. Global incidence of these tumours is 0.4-13.5 per 100,000 annually [1-5].
20–25% of the parotid gland tumors are malignant, while 40% are of submandibular glands and more than 90% are of sublingual glands [6-8]. Out of benign tumors pleomorphic adenoma is the most frequent (83%) followed by Warthins tumor. Amongst malignant tumours, mucoepidermoid carcinoma (49.3%) followed by adenoid cystic carcinoma (31.3%) are common. Parotid swelling for years is the main feature of benign, whereas malignant tumors present with pain, fixation to skin and underlying structures, cervical lymphadenopathy and facial palsy [9-11].
Several diagnostic tests including fine needle aspiration cytology (FNA) and imaging modalities have been used to answer about benign or malignant nature of the parotid mass but Magnetic resonance imaging (MRI) is considered as a non invasive modality and has high accuracy against other imaging modalities like sonography and CT scan [12]. It gives information about exact localization of the lesion, its extent, relationship with the neighboring structures, perineural spread, bone invasion and even meningeal infiltration [13]. Specific signs predictive of malignancy are hypointensity of tumor on T2 Weighted images, ill defined margins, diffuse growth, infiltration into subcutaneous tissue and lymphadenopathy. Out of them, hypointensity and ill-defined margins are highly suggestive of a malignancy [14]. The additional advantage of Magnetic resonance imaging is the visibility of retromandibular vein, hence differentiating between superficial and deep lobes of parotid gland which is important for the choice of surgical procedure [15]. These anatomical details are important because the treatment for benign parotid gland tumors is superficial parotidectomy, while total parotidectomy with or without facial nerve removal is performed for malignant tumors [16].
To best of our knowledge no local study is available till now and the international studies that have done so far shown a great variability in results. The purpose of this study was to assess the diagnostic accuracy of Magnetic resonance imaging through subjective analysis of the parotid masses imaging features to differentiate benign and malignant parotid gland tumours, so as to consider it valuable, non invasive, safe and convenient modality for early detection, surgical planning and thus obviate the role of biopsy.
Methodology
A Cross-sectional study was conducted at the Radiology Department of Lahore General Hospital, Lahore from January till July 2014. Total of 200 patients were included in the study having age ranging from 5 to 80 years, of either gender, had previously diagnosed parotid gland tumour on imaging (ultrasound or CT) or having clinical suspicion of parotid gland tumours such as parotid swelling, fixation to underlying skin and subcutaneous tissue, pain, facial palsy and cervical lymphadenopathy. Patients having contraindication to MRI, post-operative parotid gland tumours, residual or recurrent tumours and those who do not give consent were excluded from the study.
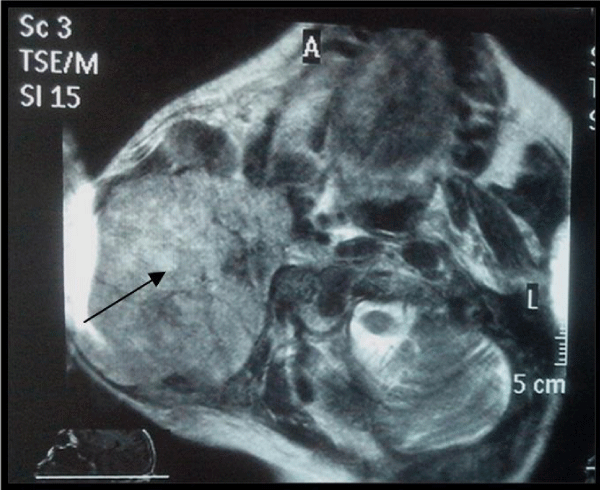
Informed consent was taken by all patients. Demographic features i.e. age and gender were recorded. MRI on a 1.5-T Philips whole body MR system using standard imaging coil was then carried out. T2-weighted, both unenhanced and contrast-enhanced T1-weighted images in the axial, sagittal and coronal projections were obtained. Image interpretation was done by single radiologist under the supervision of a senior radiologist. MRI diagnosis i.e. presence or absence of parotid gland tumor was recorded and biopsy (FNAB) was done for all the cases. Tumors showing ill-defined margins, infiltration into adjacent tissues, hypointensity on T2 and lymphadenopathy were diagnosed as malignant. Histopathological results were then recorded. The results of MRI and histopathology were then compared taking histopathology as a gold standard.
The collected data was analyzed with SPSS version 16. For quantitative data like age, mean and standard deviation were calculated. For qualitative data i.e. gender, frequencies and percentages were calculated. A 2 x 2 table was used to calculate sensitivity, specificity, positive predictive value, negative predictive value and accuracy of MRI for parotid gland tumors taking histopathology as a gold standard.
Results
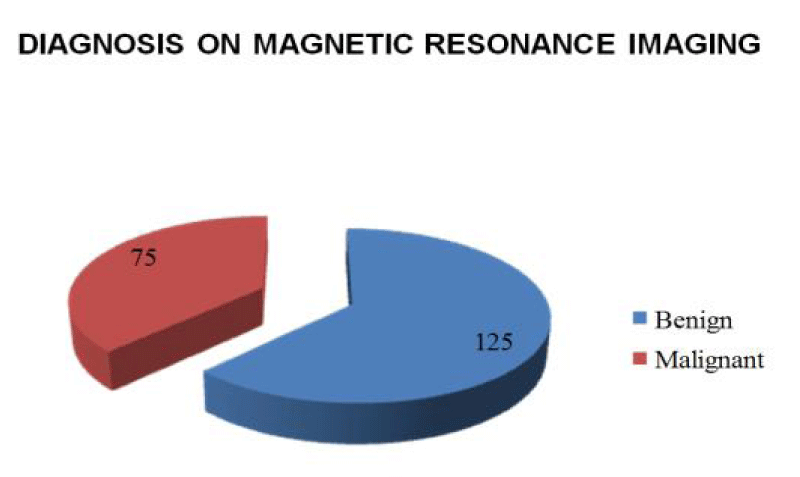
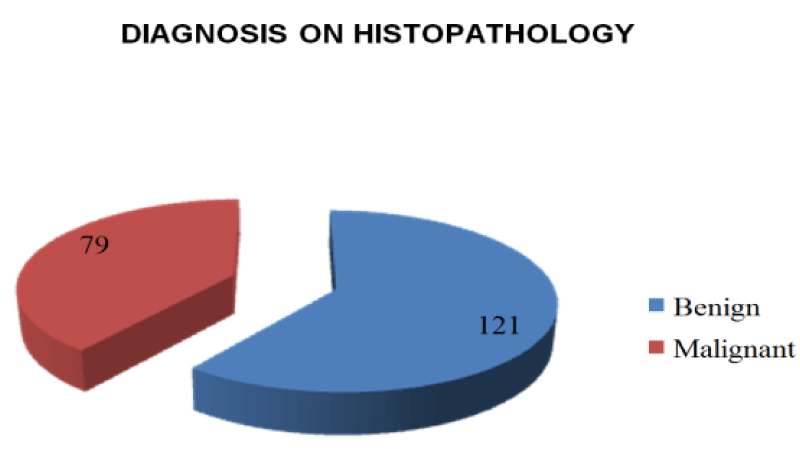
Out of 200 patients, there were 170 males and 30 females. Mean age of male and female patients was 40.27±15.04 and 40.12±12.15 years respectively. Youngest patient age was 10 years for male and 15 years for female, but the eldest patient age was same for both the genders i.e. 80 years. Based on MRI imaging characteristics 125 patients were labelled as having benign and 75 as having malignant tumours (Figure-1), while histopathological findings diagnosed 121 parotid tumours as benign and 79 as malignant tumours (Figure-2). On both the modalities i.e. on MRI and Histopathology, 113 patients were diagnosed as benign and 67 patients as having malignant parotid gland tumours (Image 1). Total of 20 patients had contradictory results, out of them 12 patients were diagnosed as benign on MRI but they were malignant on histopathology. Similarly 8 patients were diagnosed as having malignant tumour on MRI but on histopathology they were found to be having benign features (Table 1). Sensitivity, specificity, positive and negative predictive value of MRI was 90.4%, 89.33%, 93.39% and 84.41% respectively. The overall diagnostic accuracy of MRI was found to be 90% while taking results of histopathology as a gold standard.
| Table: Diagnostic Accuracy Comparison of MRI & Histopathology to Differentiate benign and Malignant Parotid Gland Tumors. | ||||
| MRI | Total | |||
| Benign | Malignant |
|||
| Benign | 113 | 8 | 121 | |
| Histopathology | Malignant | 12 | 67 | 79 |
| Total | 125 | 75 | 200 | |
Discussion
Although majority of the parotid gland tumours are benign but still it is of major importance to determine non invasive imaging method to distinguish between benign or malignant parotid gland tumours and their anatomical extent preoperatively, because it primarily influence the choice of surgical procedure i.e. superficial versus total parotidectomy [16,17].
Fine needle aspiration biopsy (FNAB) have been reported unreliable in distinguishing some specific classification of benign and malignant tumors and is prone to diagnostic error [18-20]. MRI has an advantage with respect to its noninvasiveness, lack of radiation hazard, excellent soft tissue resolution and potentially more promising imaging sequences like diffusion weighted and dynamic contrast enhanced MRI which are having more potential to detect different histological types of parotid gland tumors non-invasively [17,21-25].
Here in our study, we have inferred that the MRI can provide insight into the benign and malignant characteristics of parotid gland tumours owing to its high specificity and accuracy. It not only establishes a diagnosis but also helps in assessment of clinically questionable parotid gland lesions. Its diagnostic accuracy was found to be 90% which is comparable to the FNAB found in previous literature [19].
The study was conducted on 200 patients, which to our knowledge is the largest sample size taken so far for different studies done on the MRI of salivary gland tumors. Due to inclusion of children 5 years and onward in our study, the age range was variable. The youngest patient was of 10 years and eldest was 80 years old with a mean age of 40 years. These results are comparable with the latest available study where they found age range between 9 to 85 years and the median age of 56 years.14 Our study is also strengthening the internationally accepted view that benign parotid gland tumors are more common than malignant and that parotid gland tumors have no significant sex predilection [14,26,27].
Although variable results have been found in the international literature but overall our results are comparable to most of them. Bartels S. and colleagues retrospectively selected forty-eight patients of parotid tumors of any histology out of five hundred and eighty six (13 investigated with CT, 35 with MRI); 23 (48%) of the lesions were malignant and 25 (52%) were benign. MRI, CT, and FNA misclassified 17%, 46%, and 21% of the lesions respectively, indicating MRI being the least contributor in misdiagnosis thus comparable to our results which showed MRI misinterpreting 10 % of the patients. Sensitivity, specificity and accuracy for detecting malignant lesions on MRI and FNA were as follows: MRI (88%, 77%, 83%) and FNA (83%, 86%, 85%) respectively. The investigators concluded that imaging and FNA are comparable in their ability to correctly identify malignant parotid lesions preoperatively and that combining the two modalities yields no advantage in terms of sensitivity, specificity, and accuracy of a malignant tumor diagnosis. The results also added that MRI is the first test of choice, because it was not only as effective as FNAB at labeling the suspicion of malignancy but also provide detailed anatomical information about the extent of the primary tumor and adjacent lymph nodes [28].
Claudia Rudack et al. included 109 patients out of 582 who underwent CT or MRI and reported that MRI investigation has a sensitivity of 98%, a specificity of 52% and an accuracy of 84% [29].
Inohara H et al. conducted retrospective study and took 81 patients of parotid mass lesions (60 benign and 21 malignant) who had undergone FNAC and MRI preoperatively. They found sensitivity, specificity and accuracy of MRI for the differentiation of benign and malignant parotid mass lesions as 81%,92%, 89%, respectively. They concluded that either FNAC or MRI serve equally to predict the malignant nature of parotid mass lesions and the combination of FNAC and MRI yielded no diagnostic advantage over either modality alone [26]. These values are comparable to our results (90.4%, 89.33% and 90% respectively), but we found MRI more sensitive than this study.
29 operated parotid tumour patients were included in another study. They did conventional as well diffusion weighted sequences of MRI and calculated the effectiveness of these MRI sequences, focusing specifically on the diagnosis of the malignant tumours. Sensitivity of this examination for the diagnosis of malignancy was much lower than our results as well as previous studies i.e 90.4 % vs 57% respectively [27]. Small sample size could be interpreted as a limitation of this study.
H. Yerli et al., found MRI as 80% sensitive, 100% specific and 96% accurate in the assessment of tumour malignancy. They incorporated 25 parotid masses in the study. They also deduced from the findings that conventional MRI combined with DWI has similar diagnostic potential [30].
False-positive diagnoses, in detecting the presence of malignant parotid tumour could result in more radical surgery involving more risk to the patient who might not actually require lymph node dissection. So preoperative assessment is helpful in avoiding aggressive surgical plan as well as unnecessary surgery of inflammatory disease and possible risk to facial nerve injury [13]. In our study, 8 false positive diagnoses were made on the basis of MRI findings. Bulky mass (more than 5 cm) with compressive behaviour and/or cystic lesion were interpreted as suspicious on MRI which turned up as inflammatory lesions, cystic pleomorphic adenomas and Warthin tumours on histopathology. These errors were probably due to the large size of the tumour leading to the misinterpretation of its relation to adjacent structures and necrosis.
False-negative diagnoses, in assessing malignancy can lead to conservative surgical treatment (superficial parotidectomy without lymphadenectomy) in patients who are actually at risk of lymph node metastases [13]. In our study, 12 false negative diagnoses were made after assessing the MRI findings. They were mostly misinterpreted as benign due to small size (less than 5 cm), well defined margins and confined nature which were diagnosed as low grade mucoepidermoid carcinoma, carcinoma ex pleomorphic, acinic cell carcinoma and solitary metastasis on tissue analysis. This means that the staging errors may not be only considered to be attributable to insufficient spatial resolution of the techniques, but also to subjective interpretative mistakes. Here we have to keep it also in mind that the low grade malignancy can also have well defined margins with or without cystic component and should recommend patients for FNA in equivocal cases.
This study was not free from limitations. Only qualitative analysis of MRI was done which can generate a subjective error. Single radiologist under one supervisor interpreted the results and interobserver variability was not assessed. Although the patients included in the study were good in number but they were taken only from one tertiary care hospital and might not represent the general population.
In some studies, modern MR techniques such as Dynamic contrast enhanced MRI, Diffusion weighted MRI and MR spectroscopy have already shown promising results in depicting effectively the histological features [13,24,31,32]. So further research on larger scale from different set ups on all MR methods need to be carried out.
Conclusion
MRI has a potential role in characterization and differentiation between benign and malignant tumours of the parotid glands. It can be used as a promising non invasive diagnostic modality for pre-operative evaluation, accurate staging, proper surgical and therapeutic plan of salivary gland tumours, thus avoiding unnecessary biopsy/FNAC. Sensitivity, specificity, positive and negative predictive value of MRI was 90.4%, 89.33%, 93.39% and 84.41% respectively. The overall diagnostic accuracy of MRI was found to be 90% while taking results of histopathology as a gold standard.
References
- Lukšić I, Virag M, Manojlović S, Macan D. Salivary gland tumours: 25 years of experience from a single institution in Croatia. J Craniomaxillofac Surg. 2012; 40: e75-e81. Ref.: https://goo.gl/jzA5iN
- Wierzbicka M, Kopeć T, Szyfter W, Bem G. [Epidemiology of non-malignant salivary gland tumours based on 675 cases]. Otolaryngol Pol. 2009; 64: 281-287. Ref.: https://goo.gl/GDpW2K
- Bussu F, Parrilla C, Rizzo D, Almadori G, Paludetti G, et al. Clinical approach and treatment of benign and malignant parotid masses, personal experience. Acta Otorhinolaryngologica Italica. 2011; 31: 135. Ref.: https://goo.gl/uU7rtm
- Etit D, Ekinci N, Tan A, Altinel D, Dag F. An analysis of salivary gland neoplasms: a 12-year, single-institution experience in Turkey. Ear Nose Throat J. 2012; 91: 125-129. Ref.: https://goo.gl/sjca19
- Tian Z, Li L, Wang L, Hu Y, Li J. Salivary gland neoplasms in oral and maxillofacial regions: a 23-year retrospective study of 6982 cases in an eastern Chinese population. Int J Oral Maxillofac Surg. 2010; 39: 235-242. Ref.: https://goo.gl/pcWCSt
- Loyola A, De Araujo V, De Sousa S, De Araujo N. Minor salivary gland tumours. A retrospective study of 164 cases in a Brazilian population. Eur J Cancer B Oral Oncol. 1995; 31: 197-201. Ref.: https://goo.gl/aqRCkL
- Arshad A. Parotid swellings: report of 110 consecutive cases. Med J Malaysia. 1998; 53: 417-422. Ref.: https://goo.gl/BpFtSq
- Hom-Ross PL, Morrow M, Ljung BM. Diet and the risk of salivary gland cancer. Am J Epidemiol. 1997; 146: 171-176. Ref.: https://goo.gl/dknMoi
- Musani MA, Sohail Z, Zafar S, Malik S. Morphological pattern of parotid gland tumours. J Coll Physicians Surg Pak. 2008; 18: 274-277. Ref.: https://goo.gl/L4DXMY
- Sarfraz T, Qureshi S, Khan S, Janjua O. Clinicopathological aspects of malignant salivary gland neoplasms-a study of 150 cases at AFIP, Rawalpindi (Pakistan). 2011. Ref.: https://goo.gl/3LpNih
- Pietniczka-Załeska M, Dabrowska-Bień J. [Parotid tumors: a two-year experience of Otolaryngology Department at MSS Hospital in Warsaw]. Otolaryngol Pol. 2009; 63: 43-46. Ref.: https://goo.gl/VAbWMV
- Du L, Yuan J, Guan H, Zhang W, Liang B. [Magnetic resonance imaging for diagnosis of parotid malignant tumors and the pathological basis]. Nan fang yi ke da xue xue bao. 2010; 30: 1107-1110. Ref.: https://goo.gl/6fnNqS
- Thoeny H. Imaging of salivary gland tumours. Cancer Imaging. 2007; 7: 52-62. Ref.: https://goo.gl/4hsqxv
- Christe A, Waldherr C, Hallett R, Zbaeren P, Thoeny H. MR imaging of parotid tumors: typical lesion characteristics in MR imaging improve discrimination between benign and malignant disease. AJNR Am J Neuroradiol. 2011; 32: 1202-1207. Ref.: https://goo.gl/NwV76r
- Imaizumi A, Kuribayashi A, Okochi K, Ishii J, Sumi Y, et al. Differentiation between superficial and deep lobe parotid tumors by magnetic resonance imaging: usefulness of the parotid duct criterion. Acta Radiologica. 2009; 50: 806-811. Ref.: https://goo.gl/KRKFL9
- Ikeda M, Motoori K, Hanazawa T, Nagai Y, Yamamoto S, et al. Warthin tumor of the parotid gland: diagnostic value of MR imaging with histopathologic correlation. AJNR Am J Neuroradiol. 2004; 25: 1256-1262. Ref.: https://goo.gl/xLQzMN
- Balçık Ç, Akan H, İncesu L. Evaluating of Parotid Gland Tumours According to Diffusion Weighted MRI. Eur J Gen Med. 2014; 11: 77-84. Ref.: https://goo.gl/HKKW4U
- Alphs HH, Eisele DW, Westra WH. The role of fine needle aspiration in the evaluation of parotid masses. Curr Opin Otolaryngol Head Neck Surg. 2006;14: 62-66. Ref.: https://goo.gl/Uec8c6
- Das DK, Petkar MA, Al-Mane NM, Sheikh ZA, Mallik MK, et al. Role of fine needle aspiration cytology in the diagnosis of swellings in the salivary gland regions: a study of 712 cases. Med Princ Pract. 2004; 13: 95-106. Ref.: https://goo.gl/noMRmt
- Behzatoğlu K, Bahadir B, Kaplan HH, Yücel Z, Durak H, et al. Fine needle aspiration biopsy of the parotid gland. Diagnostic problems and 2 uncommon cases. Acta cytologica. 2003; 48: 149-154. Ref.: https://goo.gl/czzxBV
- Takashima S, Sone S, Takayama F, Maruyama Y, Hasegawa M, et al. Assessment of parotid masses: which MR pulse sequences are optimal? European journal of radiology. 1997; 24: 206-215. Ref.: https://goo.gl/rSvGz1
- Habermann C, Gossrau P, Graessner J, Arndt C, Cramer M, et al. Diffusion-weighted echo-planar MRI: a valuable tool for differentiating primary parotid gland tumors? RöFo. 2005;177: 940-945. Ref.: https://goo.gl/vVMcPf
- Motoori K, Yamamoto S, Ueda T, Nakano K, Muto T, et al. Inter-and intratumoral variability in magnetic resonance imaging of pleomorphic adenoma: an attempt to interpret the variable magnetic resonance findings. J Comput Assist Tomogr. 2004; 28: 233-246. Ref.: https://goo.gl/9kHV1m
- Eida S, Sumi M, Sakihama N, Takahashi H, Nakamura T. Apparent diffusion coefficient mapping of salivary gland tumors: prediction of the benignancy and malignancy. AJNR Am J Neuroradiol. 2007; 28: 116-121. Ref.: https://goo.gl/Df4apy
- Habermann C, Arndt C, Graessner J, Diestel L, Petersen K, et al. Diffusion-weighted echo-planar MR imaging of primary parotid gland tumors: is a prediction of different histologic subtypes possible? AJNR Am J Neuroradiol. 2009; 30: 591-596. Ref.: https://goo.gl/3QGQzM
- Inohara H, Akahani S, Yamamoto Y, Hattori K. The role of fine-needle aspiration cytology and magnetic resonance imaging in the management of parotid mass lesions. Acta oto-laryngologica. 2008; 128: 1152-1158. Ref.: https://goo.gl/rTj4gJ
- Turner F, Cohen F, Varoquaux A, Giovanni A, Duflo S, et al. [Role of diffusion weighted MR in the diagnosis of parotid tumours]. Revue de laryngologie-otologie-rhinologie. 2008; 129: 175-180. Ref.: https://goo.gl/PJXi1a
- Bartels S, Talbot JM, DiTomasso J, Everts EC, Andersen PE, et al. The relative value of fine‐needle aspiration and imaging in the preoperative evaluation of parotid masses. Head & neck. 2000; 22: 781-786. Ref.: https://goo.gl/zWH8ki
- Rudack C, Jörg S, Kloska S, Stoll W, Thiede O. Neither MRI, CT nor US is superior to diagnose tumors in the salivary glands–an extended case study. Head Face Med. 2007; 3: 19. Ref.: https://goo.gl/dP7Ynq
- Yerli H, Aydin E, Haberal N, Harman A, Kaskati T, et al. Diagnosis of common parotid tumors with magnetic resonance imaging including diffuion weighted imaging vs fine needle aspiration cytology: a comparitive study. Dentomaxillofac Radiol. 2010; 39: 349-355. Ref.: https://goo.gl/MgTori
- Alibek S, Zenk J, Bozzato A, Lell M, Grunewald M, et al. The value of dynamic MRI studies in parotid tumors. Academic radiology. 2007; 14: 701-710. Ref.: https://goo.gl/RNjkGv
- Hisatomi M, Asaumi JI, Yanagi Y, Unetsubo T, Maki Y, et al. Diagnostic value of dynamic contrast-enhanced MRI in the salivary gland tumors. Oral oncology. 2007; 43: 940-947. Ref.: https://goo.gl/2FoL9t