Abstract
Research Article
Diagnostic accuracy of Magnetic Resonance Imaging to differentiate benign and Malignant Parotid Gland Tumors
Sadia Ali, Adeena Khan*, Kiran Sarfaraz, Saba Akram, Mariam Javaid and Asma Bano
Published: 07 November, 2018 | Volume 2 - Issue 3 | Pages: 080-086
Objective: To determine the diagnostic accuracy of Magnetic Resonance Imaging (MRI) to differentiate Benign and Malignant Parotid Gland Tumors taking histopathology as gold standard.
Design: Cross sectional study.
Place and duration of study: Department of Diagnostic Radiology, Lahore General Hospital, Lahore from January till July 2014.
Methodology: 200 patients of age between 5 to 80 years of either gender with parotid gland swelling, having radiological evidence and clinical suspicion of parotid tumour like fixation to underlying skin, pain, facial palsy and cervical lymphadenopathy were taken. T1 and T2 plain and contrast enhanced 1.5 Tesla MRI unit using standard imaging coil was then carried out. Imaging was further evaluated for the presence or absence of benign or malignant parotid gland tumours using histopathology as a Gold standard. Sensitivity, specificity, positive predictive value, negative predictive value and diagnostic accuracy of MRI were taken against the gold standard.
Results: There were 170 males and 30 females having mean age of 40.27±15.04 and 40.12±12.15 years respectively. Sensitivity, specificity, positive predictive value and negative predictive value of MRI were 90.4%, 89.33%, 93.39% and 84.41% respectively. The diagnostic accuracy of MRI to differentiate benign and malignant parotid gland tumours was 90%. These results were taken against surgery histopathology as a gold standard.
Conclusion: MRI is highly accurate in differentiating malignant & benign tumours of parotid glands and can be used as an adjunct to histopathology for pre-operative evaluation of the parotid gland tumours.
Read Full Article HTML DOI: 10.29328/journal.jro.1001026 Cite this Article Read Full Article PDF
Keywords:
Magnetic resonance imaging; Parotid gland tumours; Diagnostic accuracy; Histopathology
References
- Lukšić I, Virag M, Manojlović S, Macan D. Salivary gland tumours: 25 years of experience from a single institution in Croatia. J Craniomaxillofac Surg. 2012; 40: e75-e81. Ref.: https://goo.gl/jzA5iN
- Wierzbicka M, Kopeć T, Szyfter W, Bem G. [Epidemiology of non-malignant salivary gland tumours based on 675 cases]. Otolaryngol Pol. 2009; 64: 281-287. Ref.: https://goo.gl/GDpW2K
- Bussu F, Parrilla C, Rizzo D, Almadori G, Paludetti G, et al. Clinical approach and treatment of benign and malignant parotid masses, personal experience. Acta Otorhinolaryngologica Italica. 2011; 31: 135. Ref.: https://goo.gl/uU7rtm
- Etit D, Ekinci N, Tan A, Altinel D, Dag F. An analysis of salivary gland neoplasms: a 12-year, single-institution experience in Turkey. Ear Nose Throat J. 2012; 91: 125-129. Ref.: https://goo.gl/sjca19
- Tian Z, Li L, Wang L, Hu Y, Li J. Salivary gland neoplasms in oral and maxillofacial regions: a 23-year retrospective study of 6982 cases in an eastern Chinese population. Int J Oral Maxillofac Surg. 2010; 39: 235-242. Ref.: https://goo.gl/pcWCSt
- Loyola A, De Araujo V, De Sousa S, De Araujo N. Minor salivary gland tumours. A retrospective study of 164 cases in a Brazilian population. Eur J Cancer B Oral Oncol. 1995; 31: 197-201. Ref.: https://goo.gl/aqRCkL
- Arshad A. Parotid swellings: report of 110 consecutive cases. Med J Malaysia. 1998; 53: 417-422. Ref.: https://goo.gl/BpFtSq
- Hom-Ross PL, Morrow M, Ljung BM. Diet and the risk of salivary gland cancer. Am J Epidemiol. 1997; 146: 171-176. Ref.: https://goo.gl/dknMoi
- Musani MA, Sohail Z, Zafar S, Malik S. Morphological pattern of parotid gland tumours. J Coll Physicians Surg Pak. 2008; 18: 274-277. Ref.: https://goo.gl/L4DXMY
- Sarfraz T, Qureshi S, Khan S, Janjua O. Clinicopathological aspects of malignant salivary gland neoplasms-a study of 150 cases at AFIP, Rawalpindi (Pakistan). 2011. Ref.: https://goo.gl/3LpNih
- Pietniczka-Załeska M, Dabrowska-Bień J. [Parotid tumors: a two-year experience of Otolaryngology Department at MSS Hospital in Warsaw]. Otolaryngol Pol. 2009; 63: 43-46. Ref.: https://goo.gl/VAbWMV
- Du L, Yuan J, Guan H, Zhang W, Liang B. [Magnetic resonance imaging for diagnosis of parotid malignant tumors and the pathological basis]. Nan fang yi ke da xue xue bao. 2010; 30: 1107-1110. Ref.: https://goo.gl/6fnNqS
- Thoeny H. Imaging of salivary gland tumours. Cancer Imaging. 2007; 7: 52-62. Ref.: https://goo.gl/4hsqxv
- Christe A, Waldherr C, Hallett R, Zbaeren P, Thoeny H. MR imaging of parotid tumors: typical lesion characteristics in MR imaging improve discrimination between benign and malignant disease. AJNR Am J Neuroradiol. 2011; 32: 1202-1207. Ref.: https://goo.gl/NwV76r
- Imaizumi A, Kuribayashi A, Okochi K, Ishii J, Sumi Y, et al. Differentiation between superficial and deep lobe parotid tumors by magnetic resonance imaging: usefulness of the parotid duct criterion. Acta Radiologica. 2009; 50: 806-811. Ref.: https://goo.gl/KRKFL9
- Ikeda M, Motoori K, Hanazawa T, Nagai Y, Yamamoto S, et al. Warthin tumor of the parotid gland: diagnostic value of MR imaging with histopathologic correlation. AJNR Am J Neuroradiol. 2004; 25: 1256-1262. Ref.: https://goo.gl/xLQzMN
- Balçık Ç, Akan H, İncesu L. Evaluating of Parotid Gland Tumours According to Diffusion Weighted MRI. Eur J Gen Med. 2014; 11: 77-84. Ref.: https://goo.gl/HKKW4U
- Alphs HH, Eisele DW, Westra WH. The role of fine needle aspiration in the evaluation of parotid masses. Curr Opin Otolaryngol Head Neck Surg. 2006;14: 62-66. Ref.: https://goo.gl/Uec8c6
- Das DK, Petkar MA, Al-Mane NM, Sheikh ZA, Mallik MK, et al. Role of fine needle aspiration cytology in the diagnosis of swellings in the salivary gland regions: a study of 712 cases. Med Princ Pract. 2004; 13: 95-106. Ref.: https://goo.gl/noMRmt
- Behzatoğlu K, Bahadir B, Kaplan HH, Yücel Z, Durak H, et al. Fine needle aspiration biopsy of the parotid gland. Diagnostic problems and 2 uncommon cases. Acta cytologica. 2003; 48: 149-154. Ref.: https://goo.gl/czzxBV
- Takashima S, Sone S, Takayama F, Maruyama Y, Hasegawa M, et al. Assessment of parotid masses: which MR pulse sequences are optimal? European journal of radiology. 1997; 24: 206-215. Ref.: https://goo.gl/rSvGz1
- Habermann C, Gossrau P, Graessner J, Arndt C, Cramer M, et al. Diffusion-weighted echo-planar MRI: a valuable tool for differentiating primary parotid gland tumors? RöFo. 2005;177: 940-945. Ref.: https://goo.gl/vVMcPf
- Motoori K, Yamamoto S, Ueda T, Nakano K, Muto T, et al. Inter-and intratumoral variability in magnetic resonance imaging of pleomorphic adenoma: an attempt to interpret the variable magnetic resonance findings. J Comput Assist Tomogr. 2004; 28: 233-246. Ref.: https://goo.gl/9kHV1m
- Eida S, Sumi M, Sakihama N, Takahashi H, Nakamura T. Apparent diffusion coefficient mapping of salivary gland tumors: prediction of the benignancy and malignancy. AJNR Am J Neuroradiol. 2007; 28: 116-121. Ref.: https://goo.gl/Df4apy
- Habermann C, Arndt C, Graessner J, Diestel L, Petersen K, et al. Diffusion-weighted echo-planar MR imaging of primary parotid gland tumors: is a prediction of different histologic subtypes possible? AJNR Am J Neuroradiol. 2009; 30: 591-596. Ref.: https://goo.gl/3QGQzM
- Inohara H, Akahani S, Yamamoto Y, Hattori K. The role of fine-needle aspiration cytology and magnetic resonance imaging in the management of parotid mass lesions. Acta oto-laryngologica. 2008; 128: 1152-1158. Ref.: https://goo.gl/rTj4gJ
- Turner F, Cohen F, Varoquaux A, Giovanni A, Duflo S, et al. [Role of diffusion weighted MR in the diagnosis of parotid tumours]. Revue de laryngologie-otologie-rhinologie. 2008; 129: 175-180. Ref.: https://goo.gl/PJXi1a
- Bartels S, Talbot JM, DiTomasso J, Everts EC, Andersen PE, et al. The relative value of fine‐needle aspiration and imaging in the preoperative evaluation of parotid masses. Head & neck. 2000; 22: 781-786. Ref.: https://goo.gl/zWH8ki
- Rudack C, Jörg S, Kloska S, Stoll W, Thiede O. Neither MRI, CT nor US is superior to diagnose tumors in the salivary glands–an extended case study. Head Face Med. 2007; 3: 19. Ref.: https://goo.gl/dP7Ynq
- Yerli H, Aydin E, Haberal N, Harman A, Kaskati T, et al. Diagnosis of common parotid tumors with magnetic resonance imaging including diffuion weighted imaging vs fine needle aspiration cytology: a comparitive study. Dentomaxillofac Radiol. 2010; 39: 349-355. Ref.: https://goo.gl/MgTori
- Alibek S, Zenk J, Bozzato A, Lell M, Grunewald M, et al. The value of dynamic MRI studies in parotid tumors. Academic radiology. 2007; 14: 701-710. Ref.: https://goo.gl/RNjkGv
- Hisatomi M, Asaumi JI, Yanagi Y, Unetsubo T, Maki Y, et al. Diagnostic value of dynamic contrast-enhanced MRI in the salivary gland tumors. Oral oncology. 2007; 43: 940-947. Ref.: https://goo.gl/2FoL9t
Figures:
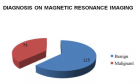
Figure 1
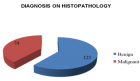
Figure 2
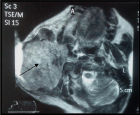
Figure 3
Similar Articles
-
Radiological evaluation of a Chondromyxoid FibromaAustin Fletcher*,Megan Mastragostino. Radiological evaluation of a Chondromyxoid Fibroma. . 2017 doi: 10.29328/journal.jro.1001008; 1: 054-059
-
Diagnostic accuracy of Magnetic Resonance Imaging to differentiate benign and Malignant Parotid Gland TumorsSadia Ali,Adeena Khan*,Kiran Sarfaraz,Saba Akram,Mariam Javaid,Asma Bano. Diagnostic accuracy of Magnetic Resonance Imaging to differentiate benign and Malignant Parotid Gland Tumors. . 2018 doi: 10.29328/journal.jro.1001026; 2: 080-086
-
Percentage of Positive Biopsy Cores Predicts Presence of a Dominant Lesion on MRI in Patients with Intermediate Risk Prostate CancerJason M Slater,William W Millard,Samuel M Randolph,Thomas J Kelly,David A Bush*. Percentage of Positive Biopsy Cores Predicts Presence of a Dominant Lesion on MRI in Patients with Intermediate Risk Prostate Cancer. . 2018 doi: 10.29328/journal.jro.1001025; 2: 073-079
-
Clinically and Radiological isolated syndrome (MS risk)Hassan Ahmed Hashem*,Yasser Hamed Mustafa,Abdelazim M Reda,Sameh Azab,Ahmed M Solaiman. Clinically and Radiological isolated syndrome (MS risk). . 2018 doi: 10.29328/journal.jro.1001020; 2: 041-046
-
Diagnostic accuracy of apparent diffusion coefficient (ADC) in differentiating low- and high-grade gliomas, taking histopathology as the gold standardRaheel Khan, Atiq-ur-Rehman Selehria, Hafsa Aquil, Atif Sheraz, Sara Khan, Najwa Zahoor, Anashia Kayani*. Diagnostic accuracy of apparent diffusion coefficient (ADC) in differentiating low- and high-grade gliomas, taking histopathology as the gold standard. . 2023 doi: 10.29328/journal.jro.1001047; 7: 013-019
-
Fatal Immune Checkpoint Inhibitor-associated Myocarditis Mimicking Infiltrative Cardiomyopathy in a 54-year-old Woman with Metastatic MelanomaHichem Sakhi*, Virgile Chevance, Laurette Kalifa, Riad Arana, Ariane Laparra, Guillaume Reverdito, Fares Ben Salem, Charles Pottier, Olivier Lambotte, Arshid Azarine*, Sondes Smaali. Fatal Immune Checkpoint Inhibitor-associated Myocarditis Mimicking Infiltrative Cardiomyopathy in a 54-year-old Woman with Metastatic Melanoma. . 2024 doi: 10.29328/journal.jro.1001063; 8: 046-050
Recently Viewed
-
Atypical Anti-GBM with ANCA Vasculitis- A Rarest of the Rare Entity: Index Case from Eastern IndiaGopambuj Singh Rathod*, Atanu Pal, Pallavi Mahato, Aakash Roy, Debroop Sengupta, Muzzamil Ahmad. Atypical Anti-GBM with ANCA Vasculitis- A Rarest of the Rare Entity: Index Case from Eastern India. J Clini Nephrol. 2024: doi: 10.29328/journal.jcn.1001139; 8: 124-126
-
Gallstone Ileus: A Rare Case of Intestinal Obstruction, Presented in a Chronic Kidney Disease Patient on HaemodialysisPulak Azad*,Yasir Sultan Rizvi,Lakshmi Kant Jha,Pranav Tyagi,Sachin Jain,Twinkle Malik. Gallstone Ileus: A Rare Case of Intestinal Obstruction, Presented in a Chronic Kidney Disease Patient on Haemodialysis. J Clini Nephrol. 2025: doi: 10.29328/journal.jcn.1001149; 9: 027-030
-
A Case of Rapidly Progressive Renal Failure with Unearthed AmyloidosisPulak Azad*,Lakshmi Kant Jha,Yasir Sultan Rizvi,Pranav Tyagi. A Case of Rapidly Progressive Renal Failure with Unearthed Amyloidosis. J Clini Nephrol. 2025: doi: 10.29328/journal.jcn.1001140; 9: 024-026
-
An Adult Case of Beta Thalassemia with Right Ventricular Outflow Tract Tachycardia: A Case ReportPrem AS,Shahanas PS,Praveen Sreekumar*,Ramaswamy NV. An Adult Case of Beta Thalassemia with Right Ventricular Outflow Tract Tachycardia: A Case Report. J Cardiol Cardiovasc Med. 2024: doi: 10.29328/journal.jccm.1001201; 9: 177-179
-
Autoantibodies in Autoimmune Addison’s Disease: Why are they Important?Maria Rosaria De Cagna, Norma Notaristefano, Maurizio Schiavone, Gianluca Palatella, Federica Ranù, Carmela Presicci, Valerio Cecinati, Marilina Tampoia*. Autoantibodies in Autoimmune Addison’s Disease: Why are they Important?. Arch Pathol Clin Res. 2024: doi: 10.29328/journal.apcr.1001042; 8: 012-015
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."